Case 20 - A 74 year old man with SOB, fever with chills, pain abdomen and chronic renal failure
A 74 year old man with SOB, fever with chills, pain abdomen and chronic renal failure.
Hi, I am R. Ramya Keerthana, 5th semester medical student.
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
Case Scenario
Nephrology Ward
DOA: 23-06-23
A 74 year old man resident of Miryalaguda came to OPD with chief complaints of:
- fever with chills since 10 days
- SOB since 10 days
- abdomen pain since 10 days
- pedal edema since 8 days.
History of Presenting Illness
- patient was apparently asymptomatic 15 years ago when he developed fever with chills associated with SOB, bilious vomiting, yellow discoloration of sclera, reduced blood pressure, reduced urine output and black blood clots in stools. He went to NIMS hospital where he was diagnosed with reanl failure and advised to undergo hemodialysis but he refused treatment and went back home.
- later he went to a local physician and was prescribed unspecified medication. His symptoms subsided after 6 months of medication and he continued them for 3 years.
- 10 days ago he developed:
1. Fever with chills, high grade, continuous, relieved on medication
2. SOB Grade 4 associated with PND and orthopnoea
3. Pain at umbilicus extending till neck, burning type, continuous, not aggravated on food intake and not relieved on medication, associated with bloating and belching.
- 8 days ago he developed bilateral pitting type pedal edema.
- no h/o headache, blurring of vision, LOC, vomiting, diarrhoea, constipation, burning micturition, reduced urine output, itching or rashes on skin.
Daily Routine
- before 10 days, he used to wake up at 6am, clean the animal shed, have breakfast (rice) and tea at 9am, then go to farm, have lunch (rice) at farm around 1-2pm, returns home at 9pm, have dinner (rice) and go to sleep.
- since 10 days, he wakes up at 7 am, has 2 idlis and tea for breakfast, stays home/goes to farm if possible, have lunch (rice) at 11am, rest, have dinner ( rice) at 8pm and go to sleep.
Past History
- n/k/c/o HTN, DM, CAD, TB, epilepsy, asthma, thyroid disorder.
- h/o of PRBC blood transfusion on 25th June.
Surgical History
- right cataract surgery 2 years ago
- left cataract surgery 1 year ago.
Personal History
- married
- farmer by occupation
- mixed diet
- decreased appetite since 10 days
- reduced sleep since 10 days
- regular bowels
- normal micturition
- no known allergies
- sutta addiction since 10 years age, 4-5/day
- chronic alcoholic since 10 years age, 1-2 glasses/ day.
Family History
- his father had left hemiplegia as a consequence of hypertension
- no DM
- no heart disease
- no tuberculosis
- no stroke
- no cancer
- no asthma
- no other hereditary diseases.
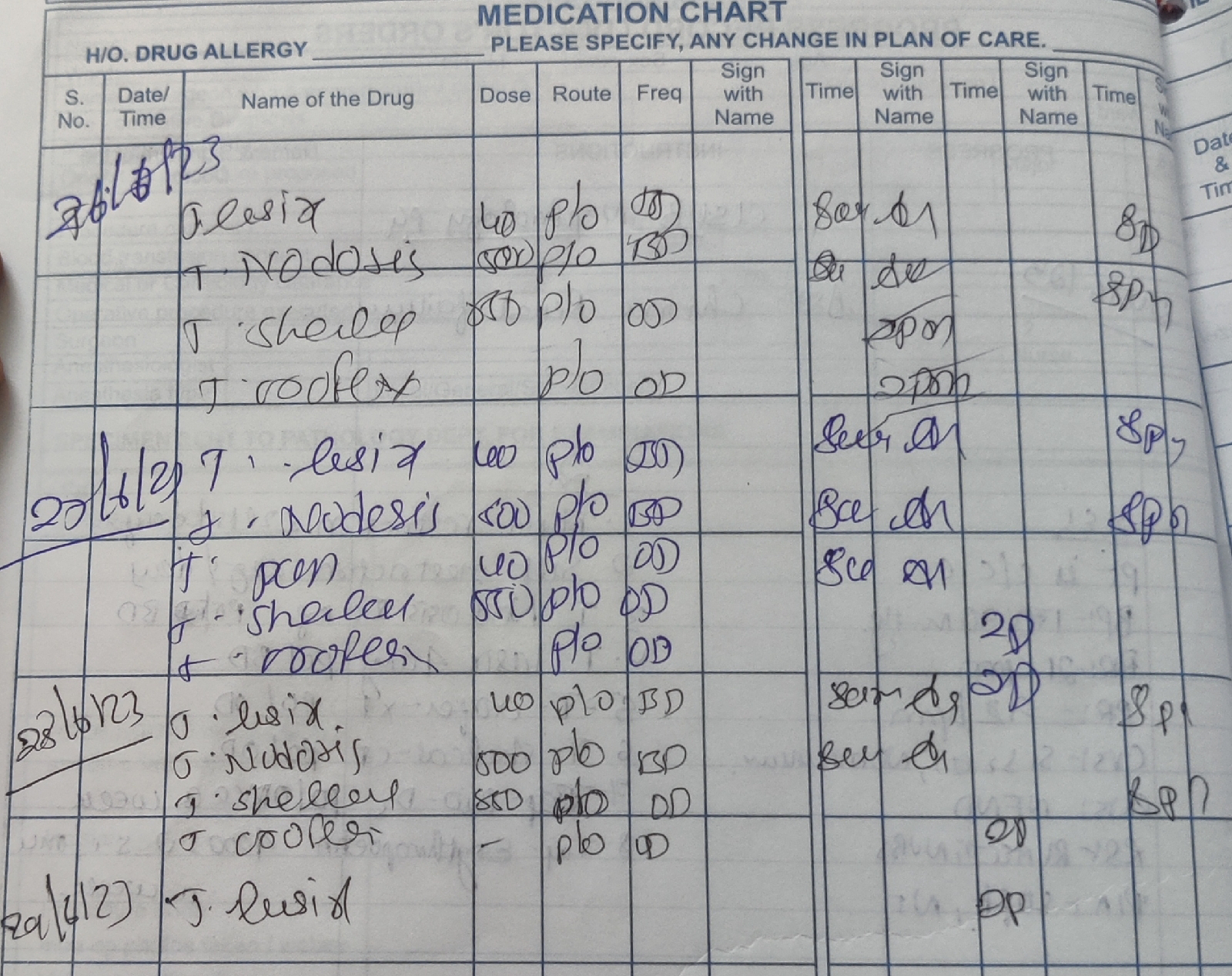
Drug History
General Examination
I have examined the patient after taken prior consent and informing the patient in the presence of a female attendant. The examination was done in both supine and sitting position in a well lit room.
- patient was conscious, coherent and cooperative
- well oriented to time and space
- well built and adequately nourished
- pallor present
- no icterus
- no cyanosis
- no clubbing of fingers
- no lymphadenopathy
- bilateral pitting type pedal edema present
- no malnutrition
- no dehydration
Vitals
- Temperature: afebrile
- Pulse rate: 66 bpm, regular rhythm, normal volume
- Respiratory rate: 18 cpm
- BP: 160/90 mm Hg
- SPO2: 98% at RA
- GRBS: 163 mg/dl
Fluid Intake and Urine Output
Total Input: ml
Total Output: ml
Fever Chart
Systemic Examination
CARDIOVASCULAR SYSTEM
Inspection :
-Shape of chest: elliptical
-No engorged veins, scars, visible pulsations
Palpation :
-Apex beat can be palpable in 5th intercostal space
- no cardiac thrills
Auscultation :
- S1,S2 are heard
- no murmurs
RESPIRATORY SYSTEM
Patient examined in sitting position
Inspection:
- Upper respiratory tract - oral cavity, nose & oropharynx appear normal.
-Chest appears Bilaterally symmetrical & elliptical in shape
- Dyspnea present
-Respiratory movements appear equal on both sides and it's abdominothoracic type.
-Trachea central in position & Nipples are in 5th Intercoastal space
-No dilated veins,sinuses, visible pulsations.
Palpation:
-All inspiratory findings confirmed
-Trachea central in position
Percussion: Resonant
Auscultation:
-Supraclavicular- (NVBS) (NVBS)
-Infraclavicular- (NVBS) (NVBS)
-Supramammary- (NVBS) (NVBS)
-Inframammary- (NVBS) (NVBS)
-Axillary- (NVBS) (NVBS)
-Infra axillary-(NVBS) (NVBS)
-Suprascapular- (NVBS) (NVBS)
-Interscapular- (NVBS)
-Infrascapular- (NVBS)(NVBS)
ABDOMEN
- shape: obese
- no tenderness
- no palpable mass
- no bruits
- no free fluid
- hernias orifices: normal
- liver: not palpable
- spleen : not palpable
- bowel sounds heard
- genitals:
- speculum examination :
- P/R examination :
CENTRAL NERVOUS SYSTEM
- conscious
- normal speech
- no neck stiffness
- no Kerning's sign
- cranial nerves: normal
- sensory : normal
- motor: normal
- reflexes: all present bilaterally
- finger nose in coordination: no
- knee heel in coordination: no
- gait: normal
Investigations
Biochemical:
USG:
2D Echo:
ECG:
Provisional Diagnosis
- CHRONIC RENAL FAILURE
Treatment
1. Fluid restriction < 2L/day
2. Salt restriction < 2gm/ day
3. T. NODOSIS 500mg PO/BD
4. T. LASIX 40mg PO/BD
5. T. OROFER- XT PO/OD
6. T SHELCAL-CT PO/OD
7. Cap. Bio D3 PO/Once a week
8. Inj. Erythropoietin 4000IU SC/Once a week
9. 2 sessions of hemodialysis on 25th and 26th of June.


















Comments
Post a Comment